FOR MEDICAL PROFESSIONALS
This section contains a captioned slide presentation displaying the spectrum of pathology encountered on the border along with Dr. Mueller’s insights and solutions for successful surgical treatment.
The descriptions are in professional jargon and the clinical images
are graphic and may be offensive to lay viewers.
 Thank you for your interest in my book. This section of the website is intended for medical professionals interested in the realities of successful remote Third World surgery. The patients and their operations depicted over several images are discussed at length in the book itself. The text is clinical and many of the photos are graphic. Lay readers may find the images disturbing and possibly offensive, but such is the reality of surgical mission work.
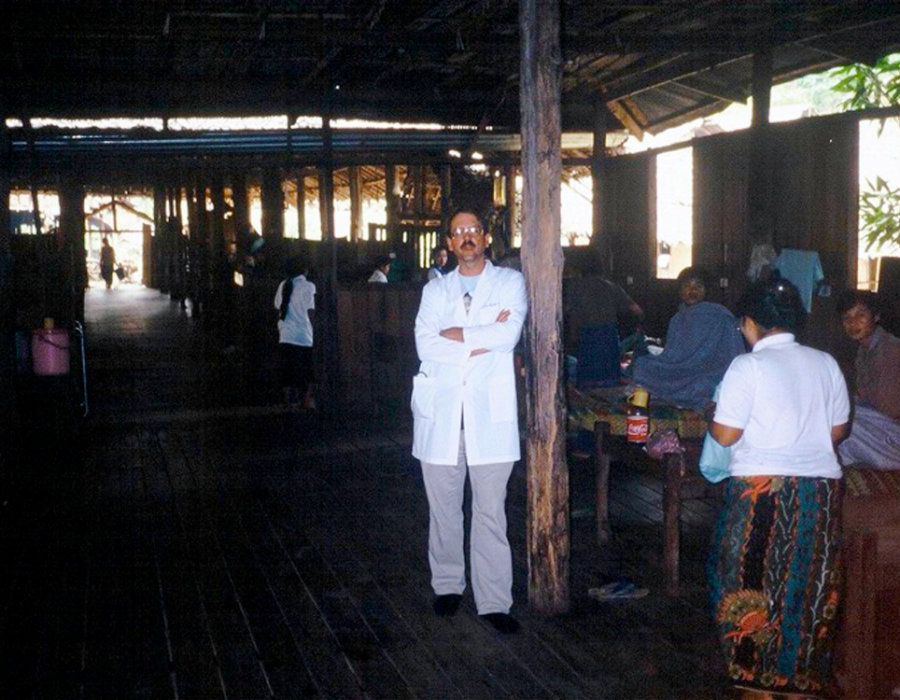
Thank you for your interest in my book. This section of the website is intended for medical professionals interested in the realities of successful remote Third World surgery. The patients and their operations depicted over several images are discussed at length in the book itself. The text is clinical and many of the photos are graphic. Lay readers may find the images disturbing and possibly offensive, but such is the reality of surgical mission work. The Karen's only hospital, located in Htoo Wah Loo, served two million people, until destroyed by the Burmese Army in 1995.
The Karen's only hospital, located in Htoo Wah Loo, served two million people, until destroyed by the Burmese Army in 1995. The nurses were uniformed, clean and professional, with access to a limited selection of medicines and supplies. They excelled at their specialty of compassionate care.
The nurses were uniformed, clean and professional, with access to a limited selection of medicines and supplies. They excelled at their specialty of compassionate care. Note the view out the OR windows. I'm harvesting a split-thickness skin graft (STSG) with a Humby knife, assisted by Karen medic Mahn Mahn.
Note the view out the OR windows. I'm harvesting a split-thickness skin graft (STSG) with a Humby knife, assisted by Karen medic Mahn Mahn. After the loss of the Htoo Wah Loo Hospital, many patients still developed problems that required life-saving surgery, like this nine-year-old boy left with a gangrenous left leg following a poisonous snakebite.
After the loss of the Htoo Wah Loo Hospital, many patients still developed problems that required life-saving surgery, like this nine-year-old boy left with a gangrenous left leg following a poisonous snakebite. Despite the lack of an adequate operating room, the Karen medics performed a successful above-knee amputation on the floor of a village hut. This photo convinced me of the need to develop a new proper surgery program for the Karens. Lives could be saved and suffering alleviated.
Despite the lack of an adequate operating room, the Karen medics performed a successful above-knee amputation on the floor of a village hut. This photo convinced me of the need to develop a new proper surgery program for the Karens. Lives could be saved and suffering alleviated. Entrance to the Mae Tao Clinic (MTC), on a Thai highway 2 km from the Burma border, the site of the new Surgery Department in 2003.
Entrance to the Mae Tao Clinic (MTC), on a Thai highway 2 km from the Burma border, the site of the new Surgery Department in 2003. All patients were housed in a single open ward. Families slept on the floor under the "beds."
All patients were housed in a single open ward. Families slept on the floor under the "beds." Due to the success of the surgery program, a new ward and operating room was built by donors in 2005.
Due to the success of the surgery program, a new ward and operating room was built by donors in 2005. The remodel included a tile floor, 25 beds, and a new operating room. During my annual missions, I performed 20 - 30 major operations, while in my absence, my trained medics performed hundreds of less complex procedures.
The remodel included a tile floor, 25 beds, and a new operating room. During my annual missions, I performed 20 - 30 major operations, while in my absence, my trained medics performed hundreds of less complex procedures. Eventually, a dropped ceiling was added as the Surgery Department's evolution continued.
Eventually, a dropped ceiling was added as the Surgery Department's evolution continued. Gauze dressings were handmade by nurses from meter-wide gauze rolls.
Gauze dressings were handmade by nurses from meter-wide gauze rolls. Families of patients also helped. All dressings were tied in small bundles, then sterilized in the autoclave.
Families of patients also helped. All dressings were tied in small bundles, then sterilized in the autoclave. Anesthesia options were local, spinal and ketamine only for general. Since I had no trained anesthesia support and virtually no diagnostic imaging, procedures in the abdominal cavity were rarely preformed.
Anesthesia options were local, spinal and ketamine only for general. Since I had no trained anesthesia support and virtually no diagnostic imaging, procedures in the abdominal cavity were rarely preformed. Karen medic Eh Tah Mwee quickly became an expert in spinal anesthesia.
Karen medic Eh Tah Mwee quickly became an expert in spinal anesthesia. The autoclave provided dry sterile gowns, drapes, towels, and washed, recycled lap sponges.
The autoclave provided dry sterile gowns, drapes, towels, and washed, recycled lap sponges. This tumor would have been removed in many patients in the States before it reached walnut size and nearly all patients when it reached lemon size.
This tumor would have been removed in many patients in the States before it reached walnut size and nearly all patients when it reached lemon size. Since my patient reported no history of trauma, and the mass did not first appear until he was a young adult, I reasoned that the underlying skull bone should be intact, without herniation of any intracranial contents. The tumor was too large for local anesthesia.
Since my patient reported no history of trauma, and the mass did not first appear until he was a young adult, I reasoned that the underlying skull bone should be intact, without herniation of any intracranial contents. The tumor was too large for local anesthesia. He accepted the risks, and I chose ketamine and a prone position, allowing airway access between shoulder and forehead pillows.
He accepted the risks, and I chose ketamine and a prone position, allowing airway access between shoulder and forehead pillows. Post op day (PO) #5 - no seromas and excellent flap healing.
Post op day (PO) #5 - no seromas and excellent flap healing. The remainder of this patient's life will now be quite different and he can now wear a baseball hat.
The remainder of this patient's life will now be quite different and he can now wear a baseball hat. 58 y/o male with a sacrococcygeal teratoma, enlarging since birth. He had no chance of ever affording an operation in Burma, even if he could find a properly-trained surgeon.
58 y/o male with a sacrococcygeal teratoma, enlarging since birth. He had no chance of ever affording an operation in Burma, even if he could find a properly-trained surgeon. My main concern was preserving his still-continent anal sphincter function, as his anal orifice was two inches down the stalk. He willingly accepted the risks.
My main concern was preserving his still-continent anal sphincter function, as his anal orifice was two inches down the stalk. He willingly accepted the risks. After a successful spinal was placed by Chief Medic Lo Kwa, my patient is prepped and the team ready to go. Time for a short prayer requesting favorable anatomy and successful healing.
After a successful spinal was placed by Chief Medic Lo Kwa, my patient is prepped and the team ready to go. Time for a short prayer requesting favorable anatomy and successful healing. The dissection is underway, heading down to the pelvic muscles.
The dissection is underway, heading down to the pelvic muscles. Further dissection with Lo Kwa retracting. So far, so good.
Further dissection with Lo Kwa retracting. So far, so good. Success! This teratoma was filled with egg-shaped sacs, some solid and some with fluid. No hair or teeth, as seen in many teratomas.
Success! This teratoma was filled with egg-shaped sacs, some solid and some with fluid. No hair or teeth, as seen in many teratomas. PO#4 appearance. A small seroma was drained on PO#2, no new reaccumulation, tight sphincter tone and no pain. Thank you God.
PO#4 appearance. A small seroma was drained on PO#2, no new reaccumulation, tight sphincter tone and no pain. Thank you God. 80 y/o grandma, six weeks since a right forearm snakebite that caused gangrene and severe pain both day and night.
80 y/o grandma, six weeks since a right forearm snakebite that caused gangrene and severe pain both day and night. PO Day #3 with no pain and no healing problems.
PO Day #3 with no pain and no healing problems. Her granddaughter was always there for her.
Her granddaughter was always there for her. She reminded me of my four daughters, and was as cute as they come. The sand colored paste on her face is actually ground bark, used both as a sunscreen and cosmetic statement.
She reminded me of my four daughters, and was as cute as they come. The sand colored paste on her face is actually ground bark, used both as a sunscreen and cosmetic statement. As with all of my patients, surgery had never been an available option, until we met.
As with all of my patients, surgery had never been an available option, until we met. My patient is comfortably asleep with IV Ketamine and no need for an endotracheal tube.
My patient is comfortably asleep with IV Ketamine and no need for an endotracheal tube. Just as I had hoped and prayed for, her tumor could be mostly finger-dissected from the surrounding normal tissue. Its few feeding blood vessels were readily seen and ligated.
Just as I had hoped and prayed for, her tumor could be mostly finger-dissected from the surrounding normal tissue. Its few feeding blood vessels were readily seen and ligated. Her benign tumor is finally where it belongs, ready for the garbage can.
Her benign tumor is finally where it belongs, ready for the garbage can. PO Day #3 - Wound closed with a subcue Vicryl suture and steri-strips.
PO Day #3 - Wound closed with a subcue Vicryl suture and steri-strips.
 His shoulder motion was significantly restricted.
His shoulder motion was significantly restricted. Now it's gone forever.
Now it's gone forever. PO Day #3 - Full shoulder ROM has returned.
PO Day #3 - Full shoulder ROM has returned. I removed many jumbo flank and abdominal wall benign masses.
I removed many jumbo flank and abdominal wall benign masses.
 This nine-year-old boy has a subcutaneous posterior thoracic lipoma.
This nine-year-old boy has a subcutaneous posterior thoracic lipoma. Without removal, this benign tumor would probably continue to enlarge, at least to softball size. In American, his tumor would already have been removed at a much younger age.
Without removal, this benign tumor would probably continue to enlarge, at least to softball size. In American, his tumor would already have been removed at a much younger age. For many years a facial cancer, type unknown, had been growing, but no cervical lymph nodes were palpable.
For many years a facial cancer, type unknown, had been growing, but no cervical lymph nodes were palpable.
 The graft is trimmed and sewn into place.
The graft is trimmed and sewn into place. The graft is stented for 5 days with a paraffin-soaked cotton ball (glycerine is used in the States), to maintain continuous contoured contact between the graft and the recipient bed.
The graft is stented for 5 days with a paraffin-soaked cotton ball (glycerine is used in the States), to maintain continuous contoured contact between the graft and the recipient bed. Karen village medics were skilled at open wound care, including debridements, but without access to skin grafting. The procedure requires a manual or electric dermatome, with sharp blades, to harvest the skin graft, and proper training. Without skin grafting, this unfortunate woman, recovering from a cooking oil burn for several months, would probably heal with thick scars and keloids, along with a frozen ankle and partially contracted knee. A skin graft will prevent these healing complications.
Karen village medics were skilled at open wound care, including debridements, but without access to skin grafting. The procedure requires a manual or electric dermatome, with sharp blades, to harvest the skin graft, and proper training. Without skin grafting, this unfortunate woman, recovering from a cooking oil burn for several months, would probably heal with thick scars and keloids, along with a frozen ankle and partially contracted knee. A skin graft will prevent these healing complications. Teaching Tint Tint the correct technique for our new Swiss electric dermatome, replacing the manual Humby knife.
Teaching Tint Tint the correct technique for our new Swiss electric dermatome, replacing the manual Humby knife.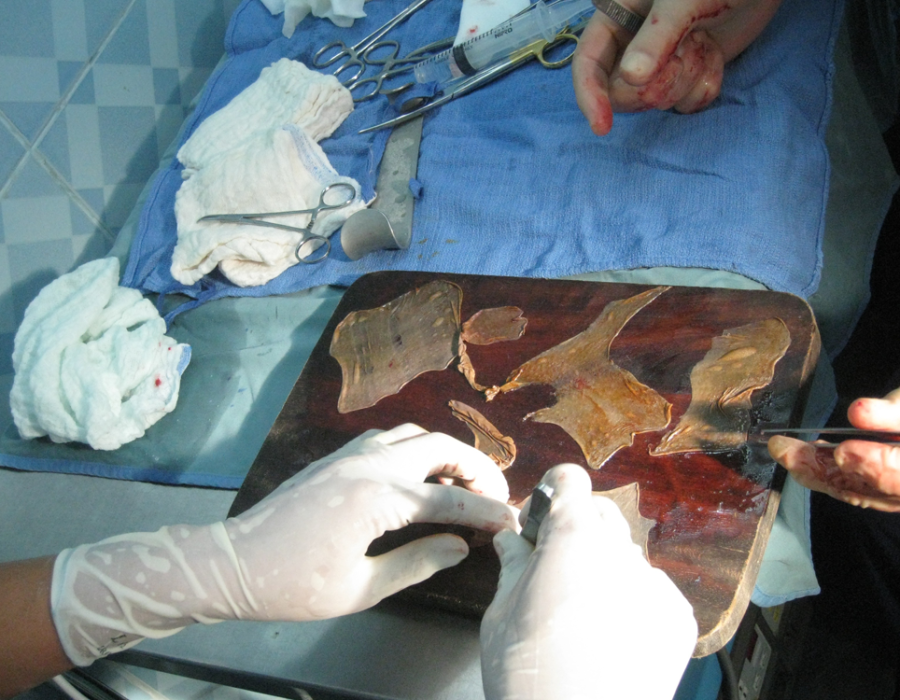 The STSG is meshed with small slits to increase its coverage area and allow for drainage of fluid from the recipient site during the early postop course. We used an autoclaved teakwood cutting board and a #15 scalpel blade for meshing.
The STSG is meshed with small slits to increase its coverage area and allow for drainage of fluid from the recipient site during the early postop course. We used an autoclaved teakwood cutting board and a #15 scalpel blade for meshing.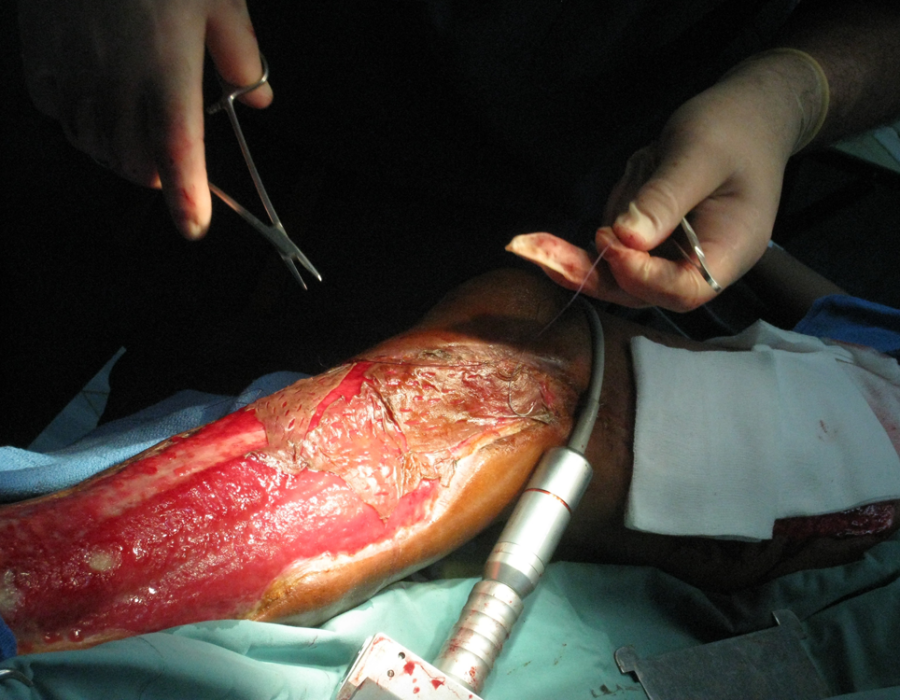 That's the new dermatome. The harvested graft pieces are trimmed to fit, then sutured to each other and the skin border.
That's the new dermatome. The harvested graft pieces are trimmed to fit, then sutured to each other and the skin border. The puzzle is nearly complete. Note the minimal donor site bleeding - the gauze was soaked with 1% lidocaine with epi.
The puzzle is nearly complete. Note the minimal donor site bleeding - the gauze was soaked with 1% lidocaine with epi. Here is another lower leg with two chronic ulcers and mature granulation tissue treated with a similar procedure.
Here is another lower leg with two chronic ulcers and mature granulation tissue treated with a similar procedure. PO#7 with 100% graft take.
PO#7 with 100% graft take. I treated many patients with excessive scarring following trauma, burns and infections that resulted in severe joint contractures. An ankle flexion contracture like this one made walking up and down muddy trails during the six-month rainy season quite a challenge.
I treated many patients with excessive scarring following trauma, burns and infections that resulted in severe joint contractures. An ankle flexion contracture like this one made walking up and down muddy trails during the six-month rainy season quite a challenge. Fortunately, after excising the scar contracture, I was pleased to see that her ankle joint had not yet froze and was able to obtain ninety degrees of extension.
Fortunately, after excising the scar contracture, I was pleased to see that her ankle joint had not yet froze and was able to obtain ninety degrees of extension. This unfortunate man had a pail full of acid thrown at him many years ago.
This unfortunate man had a pail full of acid thrown at him many years ago. His left elbow has been frozen with scar tissue and keloids ever since "healing."
His left elbow has been frozen with scar tissue and keloids ever since "healing."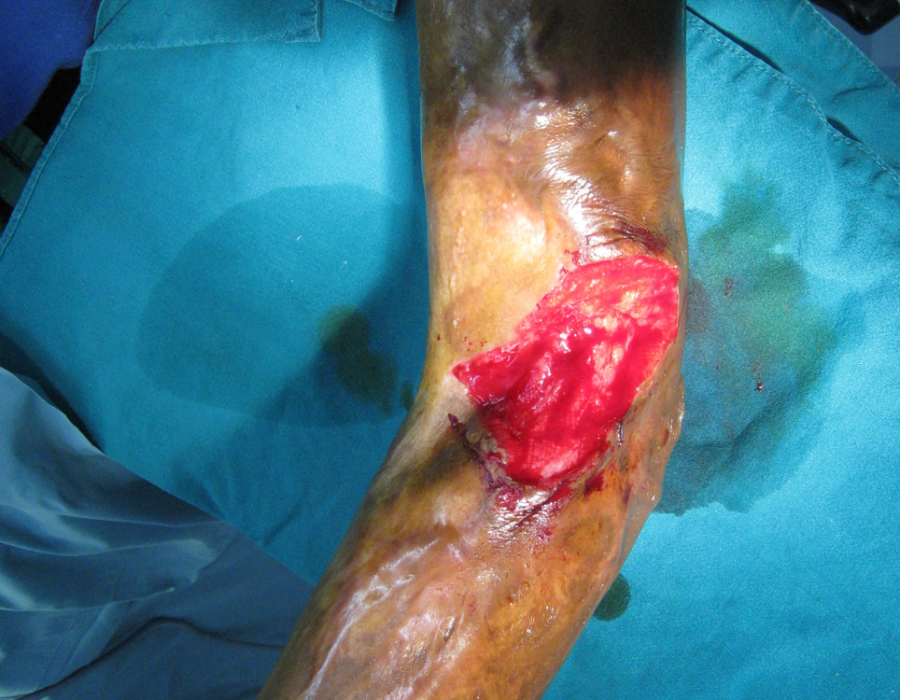 Excision of the keloid left only a remaining thirty-degree contracture, from muscle shortening and joint capsule fibrosis.
Excision of the keloid left only a remaining thirty-degree contracture, from muscle shortening and joint capsule fibrosis.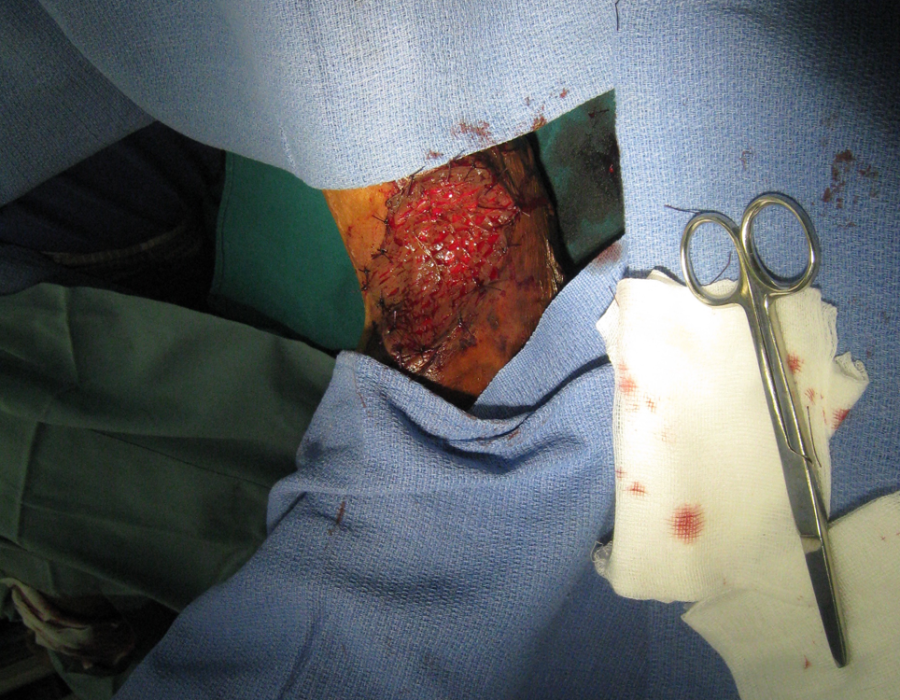 A STSG was harvested, meshed and sutured in place.
A STSG was harvested, meshed and sutured in place. One year later, physical therapy found in a refugee's day-to-day life restored complete range of motion to his left elbow.
One year later, physical therapy found in a refugee's day-to-day life restored complete range of motion to his left elbow. Leg amputations were a common operation at the MTC, thanks to land mines, poisonous snakebites, and infections.
Leg amputations were a common operation at the MTC, thanks to land mines, poisonous snakebites, and infections. I am examining this unfortunate fresh landmine victim with Eliya, Chief Medic of the Free Burma Rangers, and Lo Kwa, then Chief Medic of the MTC Surgery Department.
I am examining this unfortunate fresh landmine victim with Eliya, Chief Medic of the Free Burma Rangers, and Lo Kwa, then Chief Medic of the MTC Surgery Department. This older patient presented with a two year history of right foot gangrene, diabetes, and no pedal pulses. He needed a below knee amputation (BKA).
This older patient presented with a two year history of right foot gangrene, diabetes, and no pedal pulses. He needed a below knee amputation (BKA). Anything less would not be expected to heal, and I would not be available for another operation.
Anything less would not be expected to heal, and I would not be available for another operation. Many older male Karens were cheroot smokers and tobacco chewers, leading to significant peripherial arterial disease.
Many older male Karens were cheroot smokers and tobacco chewers, leading to significant peripherial arterial disease. Obviously, this pathology was years in the making.
Obviously, this pathology was years in the making. This patient had no place to go for a simple BKA.
This patient had no place to go for a simple BKA. Chronic osteomyletitis after a misguided procedure performed in Burma. An above knee amputation (AKA) solved his problem.
Chronic osteomyletitis after a misguided procedure performed in Burma. An above knee amputation (AKA) solved his problem. Transecting the fibula in a BKA. All were done under spinal anesthesia, with ketamine backup available if needed.
Transecting the fibula in a BKA. All were done under spinal anesthesia, with ketamine backup available if needed.
 Ligating the last bleeders during a BKA. Note the elongated posterior skin and muscle flap.
Ligating the last bleeders during a BKA. Note the elongated posterior skin and muscle flap. PO#7. Skin flaps viable with no sign of infection. Proper technique requires the incision scar to be on the anterior wall of the stump, well away from the weight-bearing cut end of the tibia.
PO#7. Skin flaps viable with no sign of infection. Proper technique requires the incision scar to be on the anterior wall of the stump, well away from the weight-bearing cut end of the tibia. Another BKA on PO#10 with a subcuticular skin closure.
Another BKA on PO#10 with a subcuticular skin closure. For years, I averaged five limb amputations per trip. My team performed many more during my absence.
For years, I averaged five limb amputations per trip. My team performed many more during my absence. Unfortunate ladies with advanced breast cancer were frequently seen. Even if they already had asymptomatic metastases, eliminating the painful, bloody, and smelling ulcer at the primary site would alleviate much suffering in their final days.
Unfortunate ladies with advanced breast cancer were frequently seen. Even if they already had asymptomatic metastases, eliminating the painful, bloody, and smelling ulcer at the primary site would alleviate much suffering in their final days. Unfortunately, the primary tumor had already invaded the poor woman's rib cage, making her a nonoperative candidate. Note the axillary metastasis.
Unfortunately, the primary tumor had already invaded the poor woman's rib cage, making her a nonoperative candidate. Note the axillary metastasis. The sad and painful natural history of breast cancer, with ascites from probable liver mets.
The sad and painful natural history of breast cancer, with ascites from probable liver mets.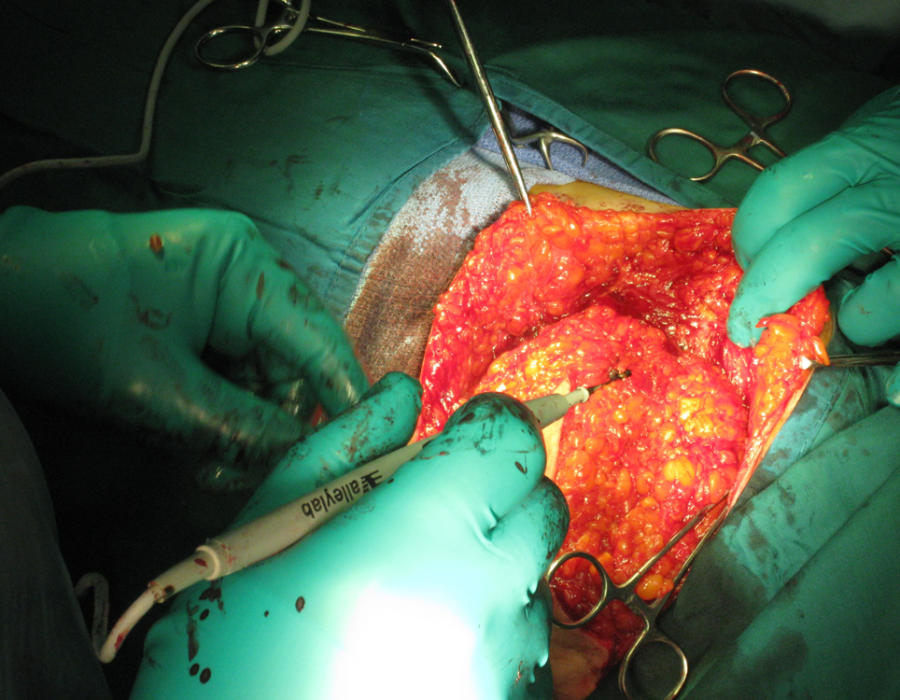 The initial dissection of medial skin flaps away from the breast to be removed.
The initial dissection of medial skin flaps away from the breast to be removed. Completed and dressed modified radical mastectomy. Along with dozens of donated boxes of suture, I brought Hemovac and bulb suction drains on each trip.
Completed and dressed modified radical mastectomy. Along with dozens of donated boxes of suture, I brought Hemovac and bulb suction drains on each trip.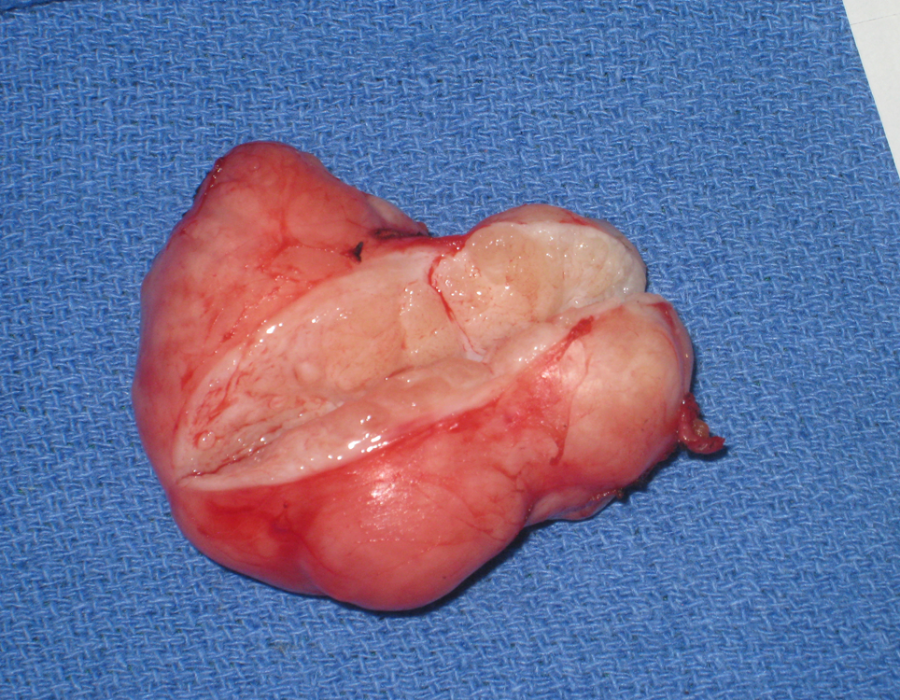 Not all breast masses were cancer. Here is a somewhat large, but otherwise typical, well-encapsulated benign fibroadenoma.
Not all breast masses were cancer. Here is a somewhat large, but otherwise typical, well-encapsulated benign fibroadenoma. That benign fibroadenoma was removed easily through a small cosmetic incision.
That benign fibroadenoma was removed easily through a small cosmetic incision. PO#7 With drains three days ago, excellent healing, and no sign of infection, my patient is ready to return to her village.
PO#7 With drains three days ago, excellent healing, and no sign of infection, my patient is ready to return to her village. What could this mass possibly be, slowly growing over several years and now tender and uncomfortable due to its size? It felt firm and rubbery, and no cervical adenopathy was palpable.
What could this mass possibly be, slowly growing over several years and now tender and uncomfortable due to its size? It felt firm and rubbery, and no cervical adenopathy was palpable. The mass was well encapsulated, deep to her mylohyoid muscle and the size of a golf ball.
The mass was well encapsulated, deep to her mylohyoid muscle and the size of a golf ball. The well encapsulated cyst contained a gray pasty filling, like found in a sebaceous cyst. I was able to completely excise the intact cyst, resulting in a cure for this patient of whatever it was. Medical mission surgery offered many surprises.
The well encapsulated cyst contained a gray pasty filling, like found in a sebaceous cyst. I was able to completely excise the intact cyst, resulting in a cure for this patient of whatever it was. Medical mission surgery offered many surprises. Through short cosmetic incisions, I removed one or two thyroglossal duct cysts on each trip.
Through short cosmetic incisions, I removed one or two thyroglossal duct cysts on each trip. Early on, I performed several subtotal thyroidectomies for huge goiters without any problems and good results. I discontinued offering the operation over concern for laryngeal spasm, since I would be the surgeon and the only one at the MTC who knew how to place an endotracheal tube. The potential risk/benefit ratio forced me to tell patients with large goiters, "I'm sorry, but I cannot help you."
Early on, I performed several subtotal thyroidectomies for huge goiters without any problems and good results. I discontinued offering the operation over concern for laryngeal spasm, since I would be the surgeon and the only one at the MTC who knew how to place an endotracheal tube. The potential risk/benefit ratio forced me to tell patients with large goiters, "I'm sorry, but I cannot help you." No amount of surgery could help this unfortunate keloid-producing patient.
No amount of surgery could help this unfortunate keloid-producing patient.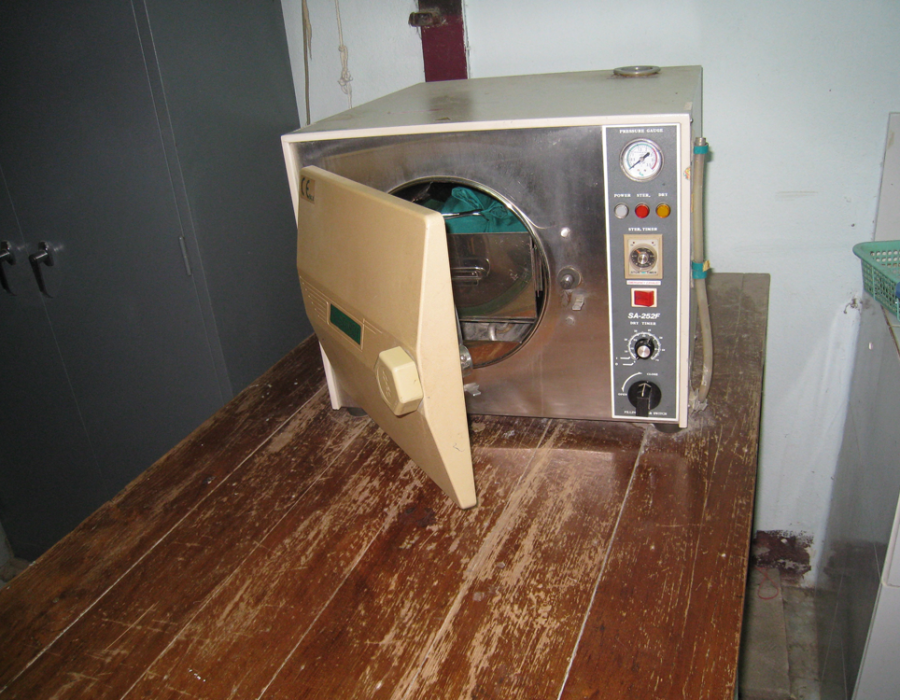 Steel instruments can be sterilized in a pressure cooker, but sterile dry linen drapes, gowns, towels and dressings require an autoclave.
Steel instruments can be sterilized in a pressure cooker, but sterile dry linen drapes, gowns, towels and dressings require an autoclave. Dry, dust-free storage kept sterilized surgery packs ready.
Dry, dust-free storage kept sterilized surgery packs ready. Electricity, from either a municipal power grid or a generator, is mandatory to power the autoclave, lights and electrocautery.
Electricity, from either a municipal power grid or a generator, is mandatory to power the autoclave, lights and electrocautery. Multiple lights eliminated shadows. An OR table with armboards allows for ready IV access, and one with adjustable height is kind on the visiting surgeon's back.
Multiple lights eliminated shadows. An OR table with armboards allows for ready IV access, and one with adjustable height is kind on the visiting surgeon's back. Donated electrocautery units are sometimes available, or a refurbished unit can be bought for $1500. I will not perform a major operation without one.
Donated electrocautery units are sometimes available, or a refurbished unit can be bought for $1500. I will not perform a major operation without one.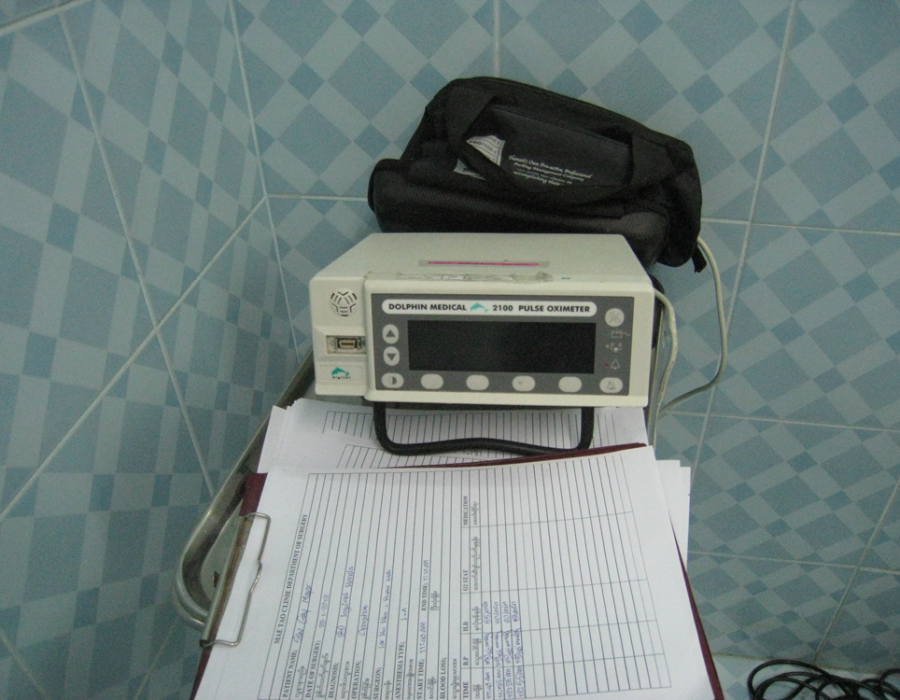 Our MTC OR unit was part of the history of pulse oximeters, c. late 1990's. A modern oximeter is a small, battery-operated clothespin-like device costing $30. I believe that this is the single most useful monitoring device for safe surgery.
Our MTC OR unit was part of the history of pulse oximeters, c. late 1990's. A modern oximeter is a small, battery-operated clothespin-like device costing $30. I believe that this is the single most useful monitoring device for safe surgery. My complete sterile backtable for a modified radical mastectomy.
My complete sterile backtable for a modified radical mastectomy. A washing machine is well worth the investment, especially if running water is available.
A washing machine is well worth the investment, especially if running water is available. My MTC medic team: Eliya, on loan from the Free Burma Rangers, Chief Surgical Medic, Lo Kwa, and Tint Tint.
My MTC medic team: Eliya, on loan from the Free Burma Rangers, Chief Surgical Medic, Lo Kwa, and Tint Tint. After Lo Kwa emigrated to the States, Eh Tah Mwee succeeded him as Chief Medic of the MTC Surgery Department.
After Lo Kwa emigrated to the States, Eh Tah Mwee succeeded him as Chief Medic of the MTC Surgery Department. This 50 y/o woman suffered from these painful nodules on her upper lateral thigh since she was a little girl. She never knew life without pain. Her problem was not described in any textbook that I was familiar with.
This 50 y/o woman suffered from these painful nodules on her upper lateral thigh since she was a little girl. She never knew life without pain. Her problem was not described in any textbook that I was familiar with. Inside her thigh I found marbles resembling calcified pieces of cauliflower, with extensive surrounding scar tissue. I excised the rocks and every bit of abnormal tissue through a four-inch incision. My Karen team explained that when she was a small child, she must have been sick with a high fever, and a village witch doctor injected her thigh with coconut milk, then took credit for her survival.
Inside her thigh I found marbles resembling calcified pieces of cauliflower, with extensive surrounding scar tissue. I excised the rocks and every bit of abnormal tissue through a four-inch incision. My Karen team explained that when she was a small child, she must have been sick with a high fever, and a village witch doctor injected her thigh with coconut milk, then took credit for her survival.